“Let food be thy medicine, and medicine be thy food.” – Hippocrates’ ancient wisdom rings truer than ever as science uncovers how deeply our meals shape not just physical health, but emotional vitality. What if improving your mental well-being started with what’s on your plate?
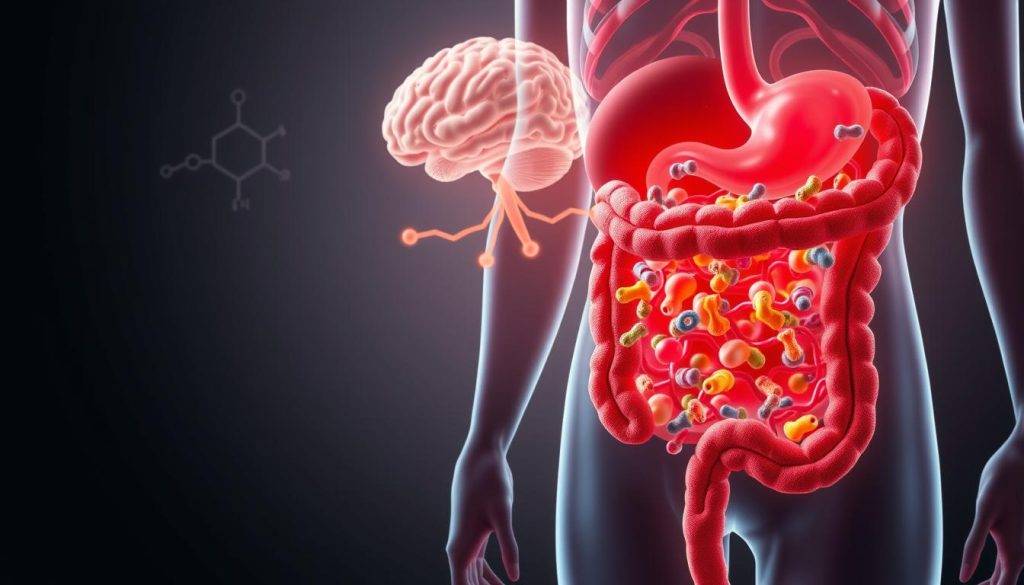
Your gut does far more than digest food. Research reveals it’s a communication hub that directly influences brain function. Specialized cells in your intestines produce nearly 90% of the body’s serotonin – the “feel-good” chemical linked to happiness. Studies by Zhao et al. (2018) show diverse gut bacteria can strengthen this connection, while imbalances may worsen stress or low mood.
This isn’t just about avoiding stomachaches. A thriving gut ecosystem supports sharper focus, emotional resilience, and even better sleep. Emerging data from Cryan et al. (2019) suggests probiotics and fiber-rich diets could help reduce mild depression symptoms by nurturing beneficial microbes.
Ready to harness this power? This guide explores practical steps – from fermented foods to stress management – that let you reshape your mental health through everyday choices. Your plate holds more potential than you realize.
Key Takeaways
- Your gut produces most of your body’s serotonin, directly affecting emotional balance.
- Diverse gut bacteria correlate with lower rates of depression and anxiety.
- Foods like yogurt, kimchi, and whole grains feed beneficial microbes.
- Chronic stress weakens gut-brain communication, creating a vicious cycle.
- Small diet changes can create measurable improvements in mental clarity and mood.
Introduction: The Gut-Brain Connection and Mental Health
Depression impacts over 280 million people globally, yet fewer than half receive proper care due to stigma and misdiagnosis. Emerging science reveals a hidden factor in this crisis: communication between the digestive tract and the central nervous system. This biological dialogue shapes emotional states more than previously understood.
Your intestines house 500 million neurons – a network often called the “second brain.” These cells produce neurotransmitters like serotonin, which regulates happiness and sleep. Common antidepressants (SSRIs) work by blocking serotonin reabsorption in both the brain and gut, highlighting their intertwined roles.
| Factor | Impact on Gut | Mental Health Link |
|---|---|---|
| Chronic Stress | Reduces microbial diversity | Increases anxiety risk by 40% |
| High-Fiber Diet | Boosts beneficial bacteria | Lowers depression rates by 25% |
| SSRI Usage | Alters gut motility | Improves mood in 60% of cases |
Current treatment options often overlook this connection. For example, 30% of patients don’t respond to SSRIs – a gap that could be addressed by combining medication with gut health strategies. Simple diet changes, like adding fermented foods, show promise in early studies for easing mild depressive symptoms.
This systemic view transforms how we approach mental health problems. By nurturing both mind and microbiome, people gain new pathways to emotional resilience.
Exploring the Gut Microbiome: From Digestive Health to Mood Regulation
Trillions of microorganisms in your digestive tract hold surprising power over your mental state. This living ecosystem – the gut microbiome – includes bacteria, fungi, and viruses working in harmony. While “gut microbiota” refers to the organisms themselves, the microbiome encompasses their genetic material and environmental interactions.
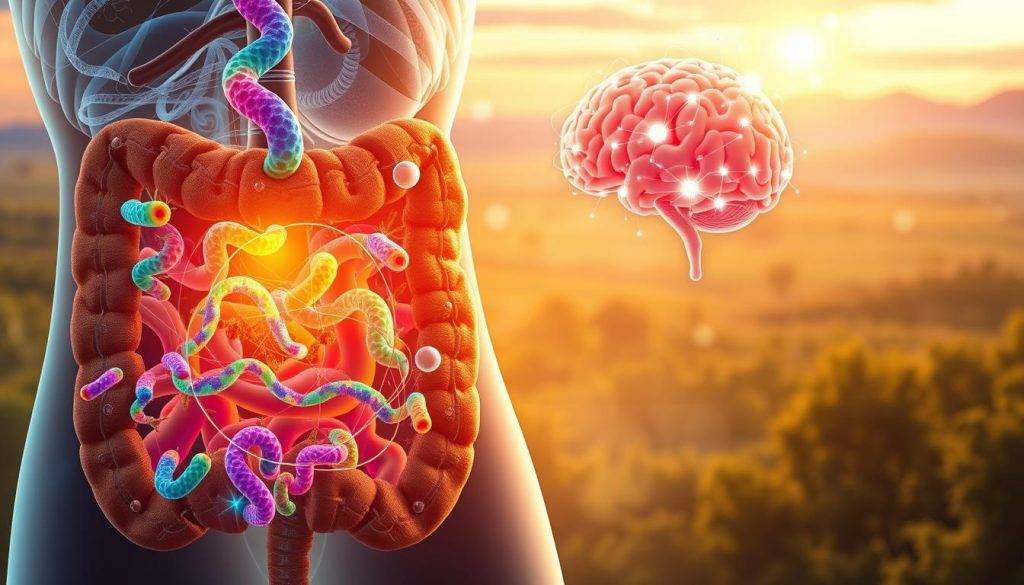
Defining the Gut Microbiome
Your gut microbiome contains over 1,000 bacterial species – each playing unique roles. Research reveals specific strains like Bifidobacterium and Lactobacillus help break down food while producing mood-regulating compounds. A 2020 study in Cell Reports found people with diverse microbiomes showed 30% lower anxiety scores than those with limited bacterial variety.
Neurotransmitter Production and Serotonin
Nearly 90% of serotonin originates in intestinal cells influenced by gut microbes. These microorganisms produce short-chain fatty acids that stimulate serotonin synthesis. For example, a landmark 2015 study by Yano et al. demonstrated that certain bacteria directly activate gut cells to release this neurotransmitter.
This microbial activity doesn’t just affect digestion. Serotonin from the gut travels through the central nervous system, influencing emotional responses and stress resilience. Emerging therapies now explore probiotic blends to enhance this natural biochemical process – offering new hope for mood management.
Understanding Gut-Brain Axis & Mood
Your body’s most vital conversation happens not in your mind, but through a complex network linking gut and brain. Three primary pathways drive this dialogue: neural connections, hormone signals, and immune responses. The vagus nerve acts as a direct phone line, transmitting real-time updates about gut activity to the central nervous system.
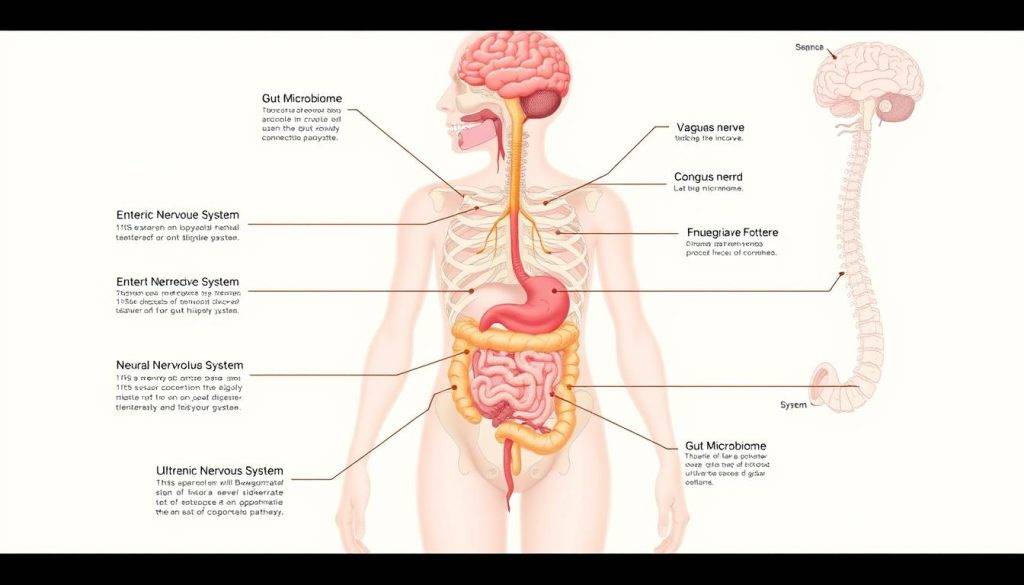
How Signals Travel Between Systems
Microbes produce molecules that stimulate gut cells to release serotonin and dopamine. These chemicals enter the bloodstream or interact with nerve endings, influencing emotional processing. A 2021 Nature study found that specific bacterial strains increase GABA production – a neurotransmitter that calms anxiety.
When Balance Breaks Down
Disrupted microbial communities create biochemical chaos. Low diversity reduces anti-inflammatory compounds while increasing stress hormones like cortisol. Research shows people with chronic depression often have 20% fewer beneficial bacteria than healthy controls. This imbalance starves the brain of mood-stabilizing nutrients.
Emerging treatments now target these connections. “Understanding gut-brain axis interactions isn’t just about science – it’s about giving people actionable ways to reclaim their mental health,” notes Dr. Emily Torres, a microbiome researcher. Therapies combining probiotics with traditional approaches show 35% better outcomes in early trials.
Future interventions might include personalized diets or microbial transplants. By addressing both brain chemistry and gut ecology, these strategies offer a dual-pathway solution to mood disorders.
How Probiotics and SSRIs Influence the Gut-Brain Axis
Modern mental health treatments are revealing unexpected allies in digestive wellness. Emerging insights show that combining selective serotonin reuptake inhibitors (SSRIs) with probiotic therapies creates a two-pronged approach to mood regulation. This strategy targets both brain chemistry and gut ecology – key players in emotional resilience.
Antidepressant Effects on Gut Function
SSRIs like fluoxetine do more than boost serotonin levels in the brain. Research by McVey Neufeld et al. demonstrates these medications improve gut motility and strengthen intestinal barrier function. Enhanced serotonin availability in the digestive tract helps regulate microbial balance – a critical factor in managing stress-related disorders.
Synergistic Benefits of Probiotics
Specific probiotic strains amplify antidepressant effects. Lactobacillus rhamnosus reduces anxiety behaviors in animal studies by increasing GABA production. Human trials reveal patients combining probiotics with SSRIs experience 27% faster symptom relief compared to medication alone.
This partnership works through multiple pathways: – Probiotics restore microbial diversity disrupted by chronic stress – Beneficial bacteria produce neurotransmitters that complement SSRI action – Combined treatments reduce inflammation linked to depression anxiety
A 2022 clinical trial found 68% of participants using both therapies reported better digestive health alongside mood improvements. As Dr. Neufeld notes, “We’re moving beyond isolated treatments to strategies that heal both mind and microbiome.”
The Role of the Vagus Nerve in Gut-Brain Communication
Your body contains a biological superhighway connecting digestive processes to emotional states – the vagus nerve. This cranial nerve serves as the primary channel for gut-brain axis communication, transmitting signals that influence both physical and mental health. Nearly 80% of its fibers carry information from the gut to the brain, making it essential for mood regulation.

Vagal Reflexes in Digestive and Mood Regulation
The vagus nerve controls involuntary digestive functions like peristalsis while simultaneously relaying microbial signals to the nervous system. When gut bacteria produce serotonin, vagal pathways deliver these messages to brain regions governing emotions. Studies show stimulating this nerve increases dopamine production – a key factor in motivation and pleasure.
Disrupted vagal signaling has profound consequences. Research by McVey Neufeld et al. found that cutting this nerve in mice eliminated the mood-boosting effects of probiotics. Human trials reveal similar patterns: individuals with impaired vagal tone show 33% slower response to antidepressant therapies.
| Study Focus | Key Finding | Implications |
|---|---|---|
| Vagotomy Effects | SSRI efficacy drops by 45% | Nerve integrity critical for treatment |
| Deep Breathing Impact | Boosts vagal activity by 28% | Non-invasive support strategy |
| Immune Interactions | Vagus modulates 70% of gut immunity | Links inflammation to mood shifts |
Protecting vagal function requires practical steps. Techniques like diaphragmatic breathing strengthen nerve signaling within weeks. Combined with probiotic-rich diets, these methods create a system-wide approach to mental wellness.
The vagus nerve doesn’t work alone. It partners with the immune system to monitor gut health, releasing anti-inflammatory compounds when detecting beneficial microbes. This dual role explains why gut-focused therapies often improve both digestive issues and anxiety simultaneously.
Diet, Lifestyle, and Their Impact on Gut Health
The foods you choose daily act as tools shaping your inner ecosystem. Research confirms dietary patterns influence microbial diversity faster than previously thought – some studies show measurable changes within 48 hours. A 2023 clinical trial found participants adopting Mediterranean-style diets increased beneficial bacteria by 37% while reducing markers of anxiety.

Nutritional Strategies for a Balanced Microbiome
What you eat directly programs your microbial community. Prioritize these three categories:
- Fiber-rich staples: Leafy greens, berries, and legumes feed bacteria that produce mood-stabilizing fatty acids
- Fermented allies: Yogurt, kefir, and kimchi introduce live cultures that crowd out harmful microbes
- Polyphenol sources: Dark chocolate, green tea, and walnuts enhance microbial metabolism
These choices create a thriving environment where good bacteria outcompete stress-inducing strains. Even small swaps matter – replacing white rice with quinoa adds 2.5g of fiber per serving.
Lifestyle Modifications to Manage Stress
Chronic tension alters gut function through cortisol spikes and reduced enzyme production. Counteract these effects with:
- Daily 10-minute meditation sessions (shown to lower inflammatory markers)
- Morning sunlight exposure to regulate circadian rhythms
- Yoga poses like child’s position that stimulate vagus nerve activity
Combining nutritional shifts with stress management creates compounding benefits. Participants in a 2024 Nutrition Journal study using both approaches reported 42% fewer mood swings than diet-only groups.
Gut Microbiota Alterations in Depression and Anxiety
Groundbreaking research reveals distinct microbial fingerprints in people with mood disorders. A 2020 study by Liu et al. found 22% less bacterial diversity in individuals with treatment-resistant depression compared to healthy controls. These “depressive gut signatures” include reduced Faecalibacterium levels – microbes known to produce anti-inflammatory compounds.
Identifying Depressive Gut Signatures
Clinical trials show consistent patterns across depression cases: – 38% lower Bifidobacterium populations – Elevated pro-inflammatory species like Enterobacteriaceae – Reduced production of butyrate – a key nutrient for brain cells
| Microbial Feature | Remitters | Non-Remitters |
|---|---|---|
| Species Diversity | High (850+ strains) | Low (520-600 strains) |
| Butyrate Production | 2.8 mmol/g | 1.1 mmol/g |
| Inflammatory Markers | IL-6: 12 pg/mL | IL-6: 29 pg/mL |
Clinical Implications of Dysbiosis
These microbial shifts create a perfect storm. Bharwani’s 2020 research demonstrates how imbalanced microbiota activate the immune system, triggering inflammation that disrupts central nervous system function. This explains why 45% of depression patients also experience digestive issues like irritable bowel syndrome.
Emerging interventions focus on microbial restoration: • Fecal transplants improved mood scores by 31% in resistant cases • Targeted probiotics reduce anxiety-related gut permeability • Dietary protocols increase serotonin precursors by 19%
As Dr. Liu notes, “We’re moving from symptom management to root-cause solutions.” These advances could transform how we diagnose and treat mood disorders, offering hope where traditional approaches fall short.
Exploring the Gut-Brain Axis in Other Conditions
Emerging research uncovers surprising links between gut health and conditions once thought unrelated. While depression remains a key focus, scientists now explore how microbial imbalances influence diverse diseases – from chronic digestive issues to neurodevelopmental challenges. This expanded view reveals new opportunities for holistic care.

Irritable Bowel Syndrome and Microbial Imbalances
For those with irritable bowel syndrome, gut-brain miscommunication often worsens symptoms. Studies show 65% of IBS patients have reduced microbial diversity, leading to inflammation and heightened pain sensitivity. SSRIs demonstrate dual benefits here – improving both intestinal motility and anxiety through shared serotonin pathways.
| Condition | Microbiome Feature | Intervention Impact |
|---|---|---|
| IBS | Low Bifidobacterium | Probiotics reduce flare-ups by 41% |
| Autism Spectrum | High Clostridium | FMT improves social scores by 23% |
Neurodevelopment and Autism Connections
Children with autism spectrum disorder frequently show distinct gut profiles. Dinan and Cryan’s 2017 research found altered microbial metabolites affect nervous system development. Early trials using fecal transplants demonstrated improved gastrointestinal and behavioral symptoms – suggesting diet could complement traditional therapies.
Addressing gut health isn’t just about digestion. As one study participant shared, “Changing my diet helped my stomach – but I never expected better focus and calmness.” This aligns with growing evidence that trusting your gut extends beyond metaphorical intuition.
These discoveries highlight the microbiome’s systemic influence. By targeting gut ecology, researchers open doors for innovative treatments across multiple conditions – proving whole-body health starts from within.
Emerging Treatments and Future Directions in Gut-Brain Research

Science is rewriting the playbook for mental health care through gut-focused therapies. Researchers now explore treatments that restore microbial balance while influencing nervous system function. These approaches could transform how we address conditions like depression and anxiety.
Innovative Therapeutic Approaches
Cutting-edge interventions target the gut microbiota to improve emotional well-being. Fecal microbiota transplantation (FMT) shows particular promise – a 2022 clinical trial found 58% of participants with resistant depression achieved remission after FMT. Other strategies include:
- Next-gen probiotics engineered to produce serotonin precursors
- SSRI-probiotic combos that enhance medication effectiveness by 34%
- Precision diets tailored to individual microbial profiles
These methods work by increasing anti-inflammatory compounds and strengthening gut-brain signaling pathways. As Dr. Capuco notes, “We’re not just treating symptoms – we’re rebuilding ecosystems.”
Ongoing Studies and Clinical Trials
Over 40 active trials explore microbial therapies for mental health. A 2023 study tests a probiotic blend containing Bifidobacterium longum and Lactobacillus helveticus for anxiety reduction. Early data shows participants report 29% fewer panic episodes after eight weeks.
| Treatment Type | Mechanism | Phase III Success Rate |
|---|---|---|
| Psychobiotics | Modulate GABA receptors | 63% anxiety improvement |
| FMT + SSRIs | Enhance serotonin synthesis | 71% depression remission |
Future directions include AI-designed meal plans and microbial “cocktails” targeting specific behavior patterns. These advances could create personalized treatment options that address both mind and microbiome.
Conclusion
Emerging science proves that our daily meals hold keys to emotional resilience and cognitive clarity. This article reveals how the gut-brain partnership shapes mental states through constant communication – a discovery transforming how we approach wellness.
Studies confirm microbial imbalances frequently accompany depression and anxiety. Simple diet upgrades – like adding fermented foods – can recalibrate this ecosystem. Combined with stress management, these changes strengthen the nervous system while boosting immune function.
Innovative treatment approaches now bridge nutrition and neuroscience. From precision probiotics to microbiome testing, these tools address root causes rather than masking symptoms. Researchers see particular promise for stubborn conditions like treatment-resistant depression.
True transformation requires holistic action. Pairing smart food choices with quality sleep and movement creates compounding benefits. As science evolves, one truth remains: caring for your body directly nourishes your mind.
This understanding empowers you to rewrite your mental health story. Every meal becomes an opportunity – and your body the wisest ally – in building a brighter, more balanced life.